Curriculum
The dynamic clinical curriculum of the General Surgery Residency Program prioritizes education over service, faculty trained to teach and hired with clear expectations of their role as facilitators of learning and an educational structure that values residents as a group and as individuals with separate learning needs and ambitions.
Clinical Rotations
Our residents receive exposure to the preoperative, operative and postoperative care for patients in the principal components of general surgery.
PGY1 (Intern Year)
- Acute Care Surgery/Trauma: Introduction to triage and care of diverse surgical patients; high-volume service with graded autonomy.
- Breast: Apprenticeship with Dr. Kevin Bethke; early exposure to breast surgery.
- Colorectal: Foundational experience in colorectal disease management.
- GI/MIS: Emphasis on anatomy, suturing, and laparoscopic skills.
- Night Float: Develop cross-cover and triage skills; exposure to emergent cases.
- Pediatrics (Lurie Children’s): Care of surgical conditions in neonates to adolescents.
- SICU Days: Critical care exposure and ICU procedures.
- Surgical Oncology (NMH & CDH): Intro to GI oncology and soft tissue malignancies.
- Thoracic: Exposure to thoracic disease management.
- Trauma (Cook County): High-penetrating trauma experience in a safety-net system.
- Vascular (NMH): Introductory exposure to vascular surgery.
PGY2
- Acute Care Surgery/Trauma: Increased responsibility in trauma triage and management.
- Gen Surg (VA): Operative experience in colorectal, foregut, and laparoscopic surgery.
- GI/MIS: Continued development of laparoscopic skills.
- Night Float: Continued development of triage and emergent care skills.
- Plastics: Increasing operative involvement and autonomy.
- SICU (Day/Night): Advanced ICU management and procedures.
- Transplant: Kidney and liver transplant management and operations.
- Vascular (NMH): Expanded operative and perioperative vascular experience.
PGY3
- Breast: Continued exposure and operative experience.
- Elective: Opportunity to pursue chosen rotation.
- Endocrine: Management of thyroid, parathyroid, adrenal, and pancreatic tumors.
- Pediatrics (Lurie Children’s): Advanced pediatric surgical care.
- Surgical Oncology (NMH & CDH): Deeper involvement in GI oncology and soft tissue surgery.
- Thoracic: Broader exposure to thoracic procedures.
- Vascular (NMH & CDH): High-volume vascular surgery experience.
- Night Float: Senior-level triage and emergent care responsibilities.
PGY4
- Acute Care Surgery/Trauma: Senior-level autonomy and leadership on a busy service.
- Colorectal: Advanced operative experience and perioperative management.
- Elective: Opportunity to pursue chosen rotation.
- Nagle Apprenticeship: One-on-one mentorship with Dr. Alex Nagle; complex general surgery.
- Night Float: Chief-level responsibilities in overnight care.
- Surgical Oncology (NMH & CDH): Senior-level involvement in complex oncologic cases.
- Transplant: Kidney and liver transplant management and operations.
PGY5 (Chief Year)
- Acute Care Surgery/Trauma: Chief-level leadership and operative autonomy.
- Colorectal: Final refinement of colorectal surgical skills.
- Gen Surg (VA): Chief responsibilities in general surgery cases.
- GI/MIS: Mastery of advanced laparoscopic techniques.
- Night Float: Oversight of junior residents and emergent surgical care.
- Rosen Apprenticeship: One-on-one mentorship with Dr. Michael Rosen; complex GI surgery.
- Surgical Oncology (NMH & CDH): Chief-level operative experience in GI oncology.
On all clinical rotations, the care of patients is ultimately the responsibility of the attending surgeon. Nevertheless, responsibilities for patient care is assigned to residents at the discretion of the attending surgeon. For residents in the junior years of the residency, such responsibilities may include observation of the preoperative treatment planning, participation in straightforward operations, monitoring of patient condition following surgery, arrangement for discharge and participating in follow-up care in the attending surgeon’s office. For residents in the senior year, responsibilities may including formulating a preoperative plan of care for approval by the attending surgeon, participating in complex operations, monitoring of patient condition following surgery, ordering appropriate tests, making recommendations for change in postoperative treatment as indicated and participating in follow-up care in the attending surgeon’s office.
Didactics
The following conferences are designed to supplement residents' self-directed learning. Residents' education time is protected to enable maximal participation and attendance.
Core Curriculum
Our Core education series is based on the This Week in SCORE curriculum. Conference preparation material is sent out from the speakers a week in advanced and residents are reminded that more readings and modules are available on the SCORE website.
Grand Rounds
This one-hour seminar provides updated on a range of cutting edge topics from our Northwestern faculty as well as numerous prominent visiting professors each year.
Skills Lab Curriculum
Skills sessions are simulations housed in our NU Simulation Center. Curricula are broken up between the intern, mid-level, and senior residents. Each session is facilitated by a designated faculty member who leads the teaching and provision of feedback within the simulation. Mentored practice sessions are also planned throughout this series to allow additional protected practice time with peer and faculty feedback. Skill acquisition is verified via "Verification of Proficiency" exams, where residents are evaluated by faculty and provided feedback on skills they have mastered and those skills in need of additional practice. New this year, we are rolling out an Intern School skills lab curriculum, designed specifically for our new interns in their first few months.
Morbidity & Mortality Conference
Each week, residents electronically report cases appropriate for presentation at M&M. A designated faculty member moderates the discussion and selects the patient cases to be presented. Each resident, having discussed the case with the faculty member prior to M&M, reviewed the appropriate literature and pertinent details, classifies the cause(s) of the patient's morbidity or mortality and presents a summary. The focus is not on blame or shame, but rather on what could have been done differently or better in an effort to best meet patients needs.
For more information please see our Morbidity & Mortality page.
Resident Seminar Series
This conference exists to include non-clinical subjects important to the development of a well-rounded surgeon. The topics correlate to the ACGME core competencies. Sample topics have included "Ergonomics in Surgery", "Financial Planning", and "Improve Based Team Training".
Feedback & Evaluation
The Resident Performance Evaluation System is designed to standardize the collection, communication and follow-up of resident performance evaluation data. It serves to clarify expectations of the residents and provides for a regular and timely formative (feedback) and summative (overall) evaluation system that meets the needs of residents and due process guidelines.
The information is used to:
- Make decisions on promotion across residency years
- Provide data to specialty boards for certification as requested
- Write letters of recommendation
- Identify areas of marginal performance and initiate corrective measures
- Note trends of weaknesses so to target needed modifications in the program.
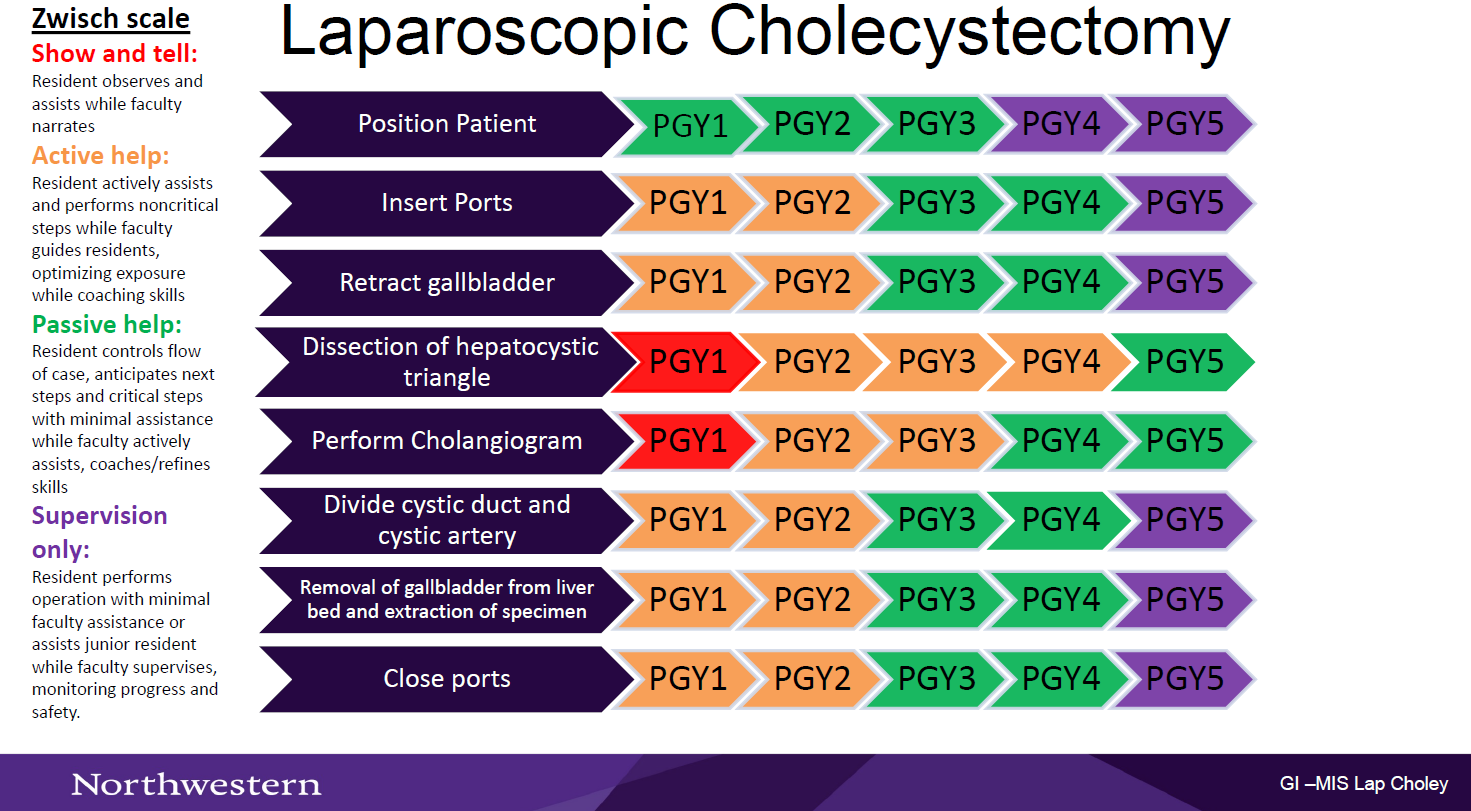
Autonomy Maps
In an effort to promote resident autonomy in the OR, we have created process maps for the most common procedures on each rotation to help create a shared mental model between attendings and learners. By creating a shared mental model of the steps for each procedure, attendings and residents will be able to do a briefing before each of these procedures to identify (1) where the resident should be at the beginning and end of each rotation, and (2) where the resident should be per their PGY year.
Here is an example of one of the autonomy maps, featuring the Zwisch scale.
Assessments
EPAs via SIMPL
The SIMPL App is used for formative assessment via ABS EPA's. The EPAs allow for constructive feedback and is given in an ongoing manner as an aid to learning. It is a convenient and reliable assessment tool that allows frequent, real-time workplace assessment and feedback.
Formative Assessment
Formative assessment or constructive feedback is given in an ongoing manner as an aid to learning. Its aim is to provide in a routine manner information that helps a resident understand what they did well and what they need to improve upon. Sources for formative assessment include the faculty, peers and self-assessment.
Summative Assessment
Summative assessment that reviews overall performance is carried out every six months. Performance data are used to assign residents an overall performance rating to help them gauge progress.
Exams
- ABSITE: The American Board of Surgery In-Training Exam.
- Mock Oral Exam: This exam is taken by fourth- and fifth-year residents every year. It is developed and administered in collaboration with two other surgery residency programs so residents are evaluated by surgical faculty they do not know to avoid potential rater bias and to mimic more closely the ABS oral exam.
Resident Research
Academic endeavors are expected of all residents throughout residency, regardless of pathway.
Our program offers the following resident research pathways:
- Academic pathway
- Resident performs research training concomitantly with clinical training
- Research electives available
- 5 years in the program
- Scholar pathway
- Resident commits to 1 year dedicated to research development following the PGY3 year
- Funding required
- 6 years in the program
- Scientist pathway
- Resident commits to 2 years dedicated to research development following the PGY3 year
- Funding required
- 7 years in the program
All residents will start on the Academic Pathway and will have the opportunity to transition to the Scientist Pathway or Scholar Pathway.
Residents will work with Dr. Karen Ho, Director of Resident Research, to develop a personal vision, identify career goals, and explore mentor options. As PGY2, residents will decide on a pathway, solidify mentor(s), and develop research projects. If pursing dedicated research time, residents will work with their mentor(s) to submit a letter of intent and apply for funding.